
A New Way to Deliver Health Care
JUNE 2018
Direct Primary Care

2 Colorado Health Institute
CHI staffers contributing to this report
• Ian Pelto, Lead Author
• Alex Caldwell
• Karam Ahmad
• Brian Clark
• Joe Hanel
• Deb Goeken
• Cliff Foster
• Chrissy Esposito
• Emily Johnson
3 Direct Primary Care 101
4 Direct Primary Care in Colorado
5 Direct Primary Care Attracts Attention of Policymakers in Colorado and Washington
6 Clinic Profi le: The Golden Stethoscope
7 Direct Primary Care Questions for Colorado
8 Two Providers, Two Perspectives
9 Conclusion
10 Endnotes
A New Way to Deliver Health Care
Direct Primary Care
On the Cover:
Dr. Amber Wobbekind examines a patient at The Golden Stethoscope, a Direct Primary Cloinic she opened in Golden in May 2017.
Photo by Brian Clark, CHI

Colorado Health Institute 3
JUNE 2018
Direct Primary Care: A New Way to Deliver Health Care
A new health care approach called Direct Primary Care will get you plenty
of face time with your doctor, free or reduced-price screenings, and often
24/7 availability by phone, text or e-mail—all for about the cost of a daily
cup of coffee.
Colorado is an enthusiastic adopter of the subscription-based health
care model, which arrived here in 2009. Today, there are about 90 or so
practices across the state, roughly 10 percent of the nation’s Direct Primary
Care clinics. They serve about 63,000 patients.
additional fees or at deep discounts. Some doctors
even make house calls, usually for an extra charge.
The goal is to establish a strong doctor-patient
relationship that focuses on preventive medicine and
results in healthier outcomes.
Specialty care and emergency services are not
included in the Direct Primary Care package, so most
patients also buy an insurance plan—usually one
with a high deductible. Some patients under the age
of 30 are eligible to buy so-called catastrophic plans,
which have low premiums and high deductibles.
Patients over 30 don’t have that option, but could
still choose from high-deductible plans.
Direct Primary Care clinics say that they save money
because they don’t have to deal with insurance
claims and other overhead costs. And with a more
predictable source of income, they don’t need to see
as many patients to keep the lights on, giving them
the ability to offer longer visits with the doctor.
Physicians told the Colorado Health Institute (CHI)
that traditional primary care providers typically
spend about 12 to 15 minutes with each patient for
routine visits, but that Direct Primary Care visits are
often between 30 and 60 minutes and can include
integrated behavioral health care screenings in
some clinics.
Each Direct Primary Care provider maintains a
panel of 600 to 800 patients, compared with
approximately 2,300 patients in the panel of a
traditional primary care provider (See Table 1).
In some respects, Direct Primary Care users are
Proponents say the model’s advantages over
traditional primary care include longer appointments
with doctors, a focus on preventive care, and the ability
to forge stronger relationships between providers and
their patients. Many doctors who have switched report
increased job satisfaction. Some advocates believe it is
the future of primary care.
Skeptics, however, worry that the model creates a two-
tiered system: one for those who can afford to bankroll
their primary care out of their own pocket in addition
to their insurance plan and another for people with
lower incomes who rely on public insurance or might
not be able to take on an extra monthly bill.
This paper explores Direct Primary Care, analyzes
how it might solve some of the problems plaguing
the health care system, looks at policy options, and
takes you inside one of the state’s Direct Primary Care
practices.
Direct Primary Care 101
Direct Primary Care is a simple concept: a fl at fee
covers many basic health care services from a primary
care doctor.
Patients pay a monthly fee, generally about $85.
1
Direct
Primary Care practices don’t accept health insurance.
The menus of services in Direct Primary Care clinics
vary. The fee generally covers at least monthly patient
visits, and in some cases also covers unlimited visits
or 24-hour access. Prescriptions, lab tests, X-rays,
and minor procedures are generally offered without
4 Colorado Health Institute
managing their health like they would manage their
car maintenance. Routine work like oil changes and
tune ups are paid out-of-pocket, with insurance
covering bigger ticket items such as collisions or hail
damage. Patients use Direct Primary Care for routine
health services and turn to insurance to help pay for
expenses such as surgery and hospital stays.
Under Colorado state law, Direct Primary Care
providers cannot contract with Medicaid
or its members.
2
That means they are
not allowed to bill Medicaid. In addition,
Medicaid members can’t pay out-of-pocket
for Direct Primary Care services.
Direct Primary Care is often confused with
a high-cost subscription model known
as Concierge Care that caters to wealthy
consumers. Concierge Care also charges
a monthly subscription rate for services like 24/7
provider access. The difference is Concierge Care
providers traditionally charge insurers on top of the
subscription cost. Most concierge practices charge
around $200 per month for unrestricted access to
a physician, though some high-end Los Angeles
practices charge as much as $30,000 per month for
24-hour access, spa services and exercise sessions.
3,4
Direct Primary Care in Colorado
Colorado had roughly 90 Direct Primary Care clinics
as of May 2018, according to DPCFrontier.com, an
industry support website founded by Direct Primary
Care advocate Dr. Phil Eskew. (See Map 1). Most of
the clinics are located along the Front Range near
cities, including Boulder, Denver and Fort Collins. But
there are clinics as far northeast as Sterling in Logan
County and as far west as Grand Junction.
And interest is growing.
For example, the state of Colorado
is offering employees who have
UnitedHealthcare insurance the option to
become a member of Paladina Health, a
Direct Primary Care company with 10 offi ces
from Pueblo to Boulder.
11,12
CHI estimates that 86 percent of Coloradans — more
than 4.6 million people — live within a 15-minute drive
of a Direct Primary Care clinic.
The state accounts for only two percent of the U.S.
population, yet it has roughly 10 percent of the
nation’s 845 Direct Primary Care clinics.
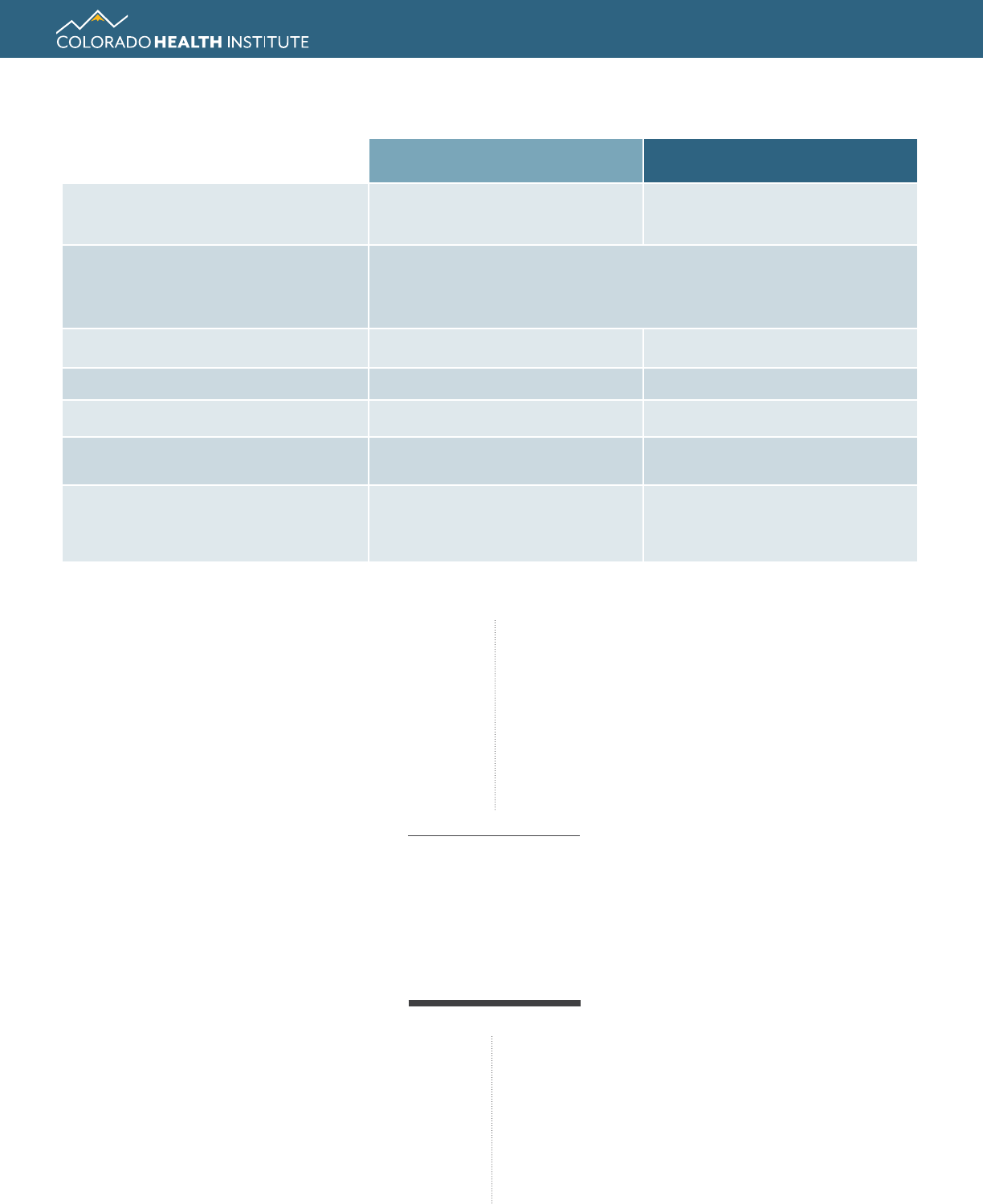
Table 1. Comparing Direct Primary Care with Traditional Primary Care
Direct Primary Care Traditional Primary Care
What is it?
Subscription service
for primary care
Accessing primary care providers in
your insurance network
Services
Both provide a variety, including treating illness, screenings,
immunizations, chronic disease management. Direct Primary Care
often offers more care management and high-touch services.
Estimated Patients Served in Colorado 63,000
5
3,228,000
6
Bills Insurance for Services? No Yes
Average Length of Patient Visit 30 to 60 minutes 12 to 15 minutes
Average Patient Panel Size per
Provider
600 to 800 patients
7
2,300 patients
8
Monthly Cost to Patients
$85 average monthly
premium
9
*
$368.81 average monthly
premium for second lowest-cost
silver plan in Front Range counties
10
* Note: This includes only primary care and does not cover services such as surgery and hospitalization, which are commonly covered by
traditional insurance plans.
86%
of Coloradans
live within a 15-minute
drive of a Direct
Primary Care clinic
Colorado Health Institute 5
JUNE 2018
Direct Primary Care: A New Way to Deliver Health Care
Direct Primary Care clinics were well-
established in Colorado when lawmakers
passed legislation in 2017 exempting them
from state insurance regulations.
13
So,
growth might be driven less by friendly
legislation and more by an entrepreneurial
spirit and a supportive network of
physicians who paved the way.
Direct Primary Care clinics are not required
to report data to the government about
which services they offer, how much they
charge and how many patients they
serve. As a result, little is known about the
average income, health status, age and
ethnicity of their patients and how they
might differ from those in more traditional
primary care practices.
Proponents say relief from administrative
paperwork is among the reasons Direct
Primary Care clinics are attractive to
providers. But the lack of government
oversight worries those who would prefer
to keep a closer eye on the quality and
delivery of health care services.
Direct Primary Care: A History
Direct Primary Care debuted on the health care
scene around 2000 with a clinic called Qliance in
Seattle. The clinic proved successful, attracting
the attention—and investments of around
$6 million—from Amazon founder Jeff Bezos,
computer guru Michael Dell, comedian Drew
Carey and other venture capitalists.
But Qliance closed in 2017 following an
unsuccessful pilot program with Washington’s
Medicaid program. Qliance said it assumed more
fi nancial risk than it could manage for its patient
population. Ultimately, it failed due to political
pushback on the program.
Dr. Clint Flanagan, a primary care and emergency
room physician, opened Colorado’s fi rst Direct
Primary Care practice near Boulder in 2009.
Today, his Nextera Healthcare clinics are located
in more than 30 places in Colorado, Nebraska,
Washington D.C., and Florida.
14
Direct Primary Care Attracts
Attention of Policymakers in
Colorado and Washington
In 2017, Colorado joined 27 other states with laws
related to Direct Primary Care.
House Bill 17-1115, a victory for Direct Primary Care
advocates, exempts Direct Primary Care from state
regulation, meaning that clinics are not subject to
requirements for claims data reporting and price
transparency. The law does prohibit Direct Primary
Care clinics from discriminating against patients based
on health status, age, citizenship, race, disability and
other factors. While this means Direct Primary Care
clinics don’t have to deal with the administrative
burden of reporting metrics, it worries some observers
who would rather have a better understanding of the
care being provided in these clinics.
Several federal laws proposed in 2017 sought to
overturn a tax rule that prevents the use of health
savings accounts for Direct Primary Care. As of June
2018, none have passed.
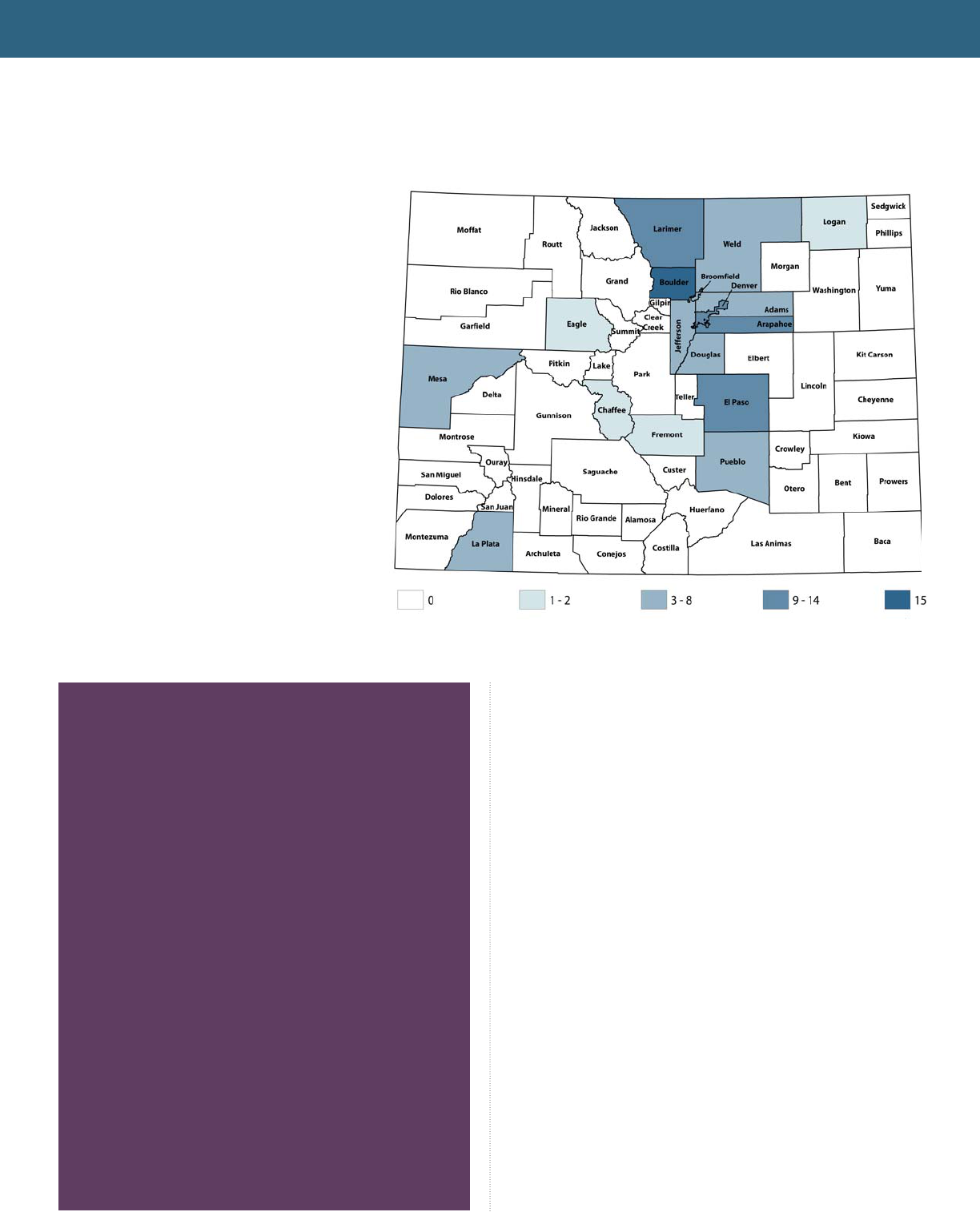
Map 1. Many Direct Primary Care Clinics Are Located
Along the Front Range
Number of Direct Primary Care Clinics by County, 2018.
Source: CHI’s analysis of data from DPCFrontier.com
6 Colorado Health Institute
“As soon as I heard that I thought, ‘This is it. This is how
it’s going to work for me as a doctor,’ ” she said.
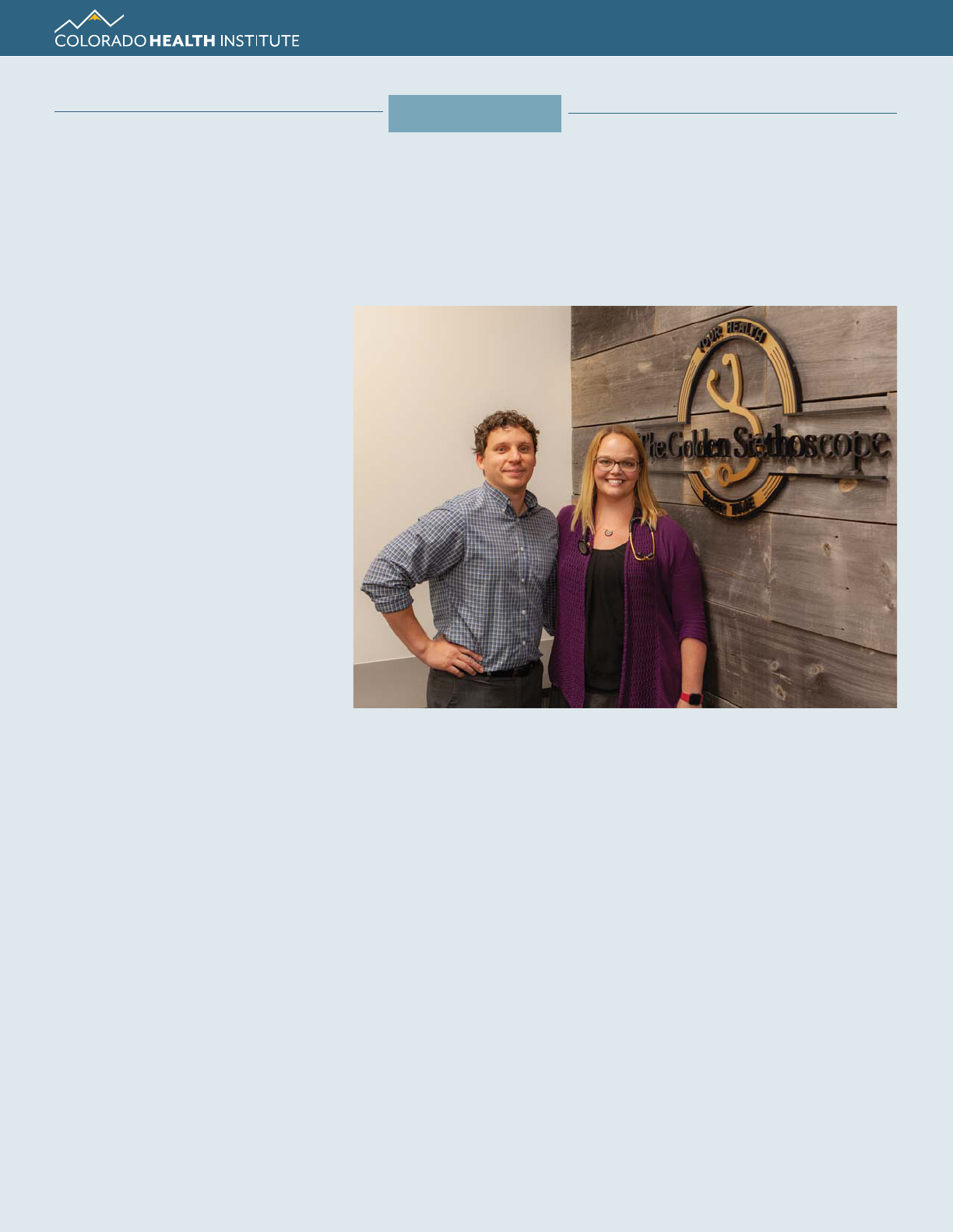
Wobbekind, a Colorado native, opened her Golden
Stethoscope clinic in Golden last May. Owning her own
practice gives her the freedom to provide health care
and spend time getting to know her patients, she says.
Monthly membership at The Golden Stethoscope costs
between $90 and $115 a month, depending on age.
Patients receive up to 20 visits per year. There are no
copays, and patients are told about any additional
costs up-front.
“Anything I can do with my brain and my two
hands and the equipment in the offi ce is part of it,”
Wobbekind said.
Dr. Amber Wobbekind and her husband, Daniel Battersby,
operate The Golden Stethoscope in Golden. A desire to spend
more quality time treating patients drove Wobbekind to open
the Direct Primary Care clinic.
Photo by Brian Clark, CHI
The Golden Touch
Physician Creates Practice That Values Patients’ Health and Time
M
ost mornings, Dr. Amber
Wobbekind was already running
behind before the coffee had fi nished
brewing at Denver Health.
She and the other primary care
doctors, faced with a full slate of
patients, scheduled 12 appointments
per half day starting at 8 a.m. To have
even a fi ghting chance at making the
appointment math work, they could
afford to spend about 15 minutes with
each patient, including time to fi ll out
charts and paperwork.
Wobbekind, a big believer in getting
to know her patients, routinely spent
30 to 40 minutes in each visit, not
including charts and paperwork. She
brought home an additional three to
four hours of that work each night.
“In the primary care system the way it is, that’s not
functional,” she said. “You can’t be a person who
does that.” Her supervisors offered to provide her with
effi ciency training.
Realizing the traditional primary care model was not
working for her, Wobbekind began exploring other
options. Everywhere she looked, however, she found
the same type of model: Too many patients, not
enough time.
Her husband, Daniel Battersby, brought up the concept
of Concierge Care. After initially bristling at the idea
because of its reputation as high-cost care for the
wealthy, Wobbekind found herself becoming intrigued
by Direct Primary Care, “the inexpensive sibling of
Concierge Care.”
After listening to a podcast by two Direct Primary Care
doctors from Wichita, Kansas, she was sold.
CLINIC PROFILE
Colorado Health Institute 7
JUNE 2018
The absence of tight time constraints allows
Wobbekind, an internal medicine doctor, to spend
time doing more things she is trained to do but
never had the time to do in a traditional primary
care facility. And more importantly, the clock does
not start ticking the moment Wobbekind enters
the exam room. She brings a laptop along, but
doesn’t open it unless necessary. “I don’t want the
computer to be what I’m talking to,” she said.
Appointments at the Golden Stethoscope are
scheduled for an hour. Most patients don’t need
that much time, but having it available eliminates
the feeling of being
rushed through the
doctor’s offi ce.
Wobekind is available at
all hours, but the impact
of an occasional late-
night call is lessened by
the familiarity she has
with her patients. “I’m on
call, but it’s my patients
calling me,” she said. “I
know what’s going on,
and I don’t have to pull up a medical chart or
fi gure out who they are.”
Wobbekind treats about 100 patients now, but
her goal is 700 patients. With that growth, she
envisions adding more providers, including
another doctor, a physician’s assistant, a
behavioral health specialist and an acupuncturist.
Each would maintain their own group of patients
to ensure strong relationships.
“There are liabilities and pieces to fi gure out, but
the plan is it will be a very integrated environment
for patients to take advantage of all those things,”
she said.
For now, Wobbekind enjoys operating a practice,
“where both your health and your time are
golden,” as it states on her business cards.
“I believe the only way to do primary care
sustainably for me is Direct Primary Care,” she
said. “I think it’s worth the money, but I want my
patients to think it’s worth it.”
Direct Primary Care Questions
for Colorado
The Direct Primary Care model of health care could have
benefi ts for Coloradans and their health care pro
viders
— from longer, richer visits to reduced red tape. But
those benefi ts could come at a price. Opponents are
concerned that Direct Primary Care could undercut
traditional health care providers and make it more
diffi cult for some patients to get care.
CHI suggests these questions for policymakers to
consider when it comes to Direct Primary Care:
Could Direct Primary Care improve access to primary
care in Colorado?
More than 800,000 Coloradans reported in 2017 that
they couldn’t get an appointment with a doctor’s offi ce
or clinic when they needed it.
15
Others said they didn’t
get care because the provider was too far away, they
couldn’t get child care, or they couldn’t take time off
work, among other reasons.
In those cases, Direct Primary Care presents an
attractive alternative—for those who can afford it. The
monthly fee simplifi es health care costs and offers
appointment and service fl exibility to access care when
and where a patients needs it with services like mobile
clinics and house calls.
Will Direct Primary Care hurt Colorado’s health care
workforce?
Critics worry that a growing number of Direct Primary
Care practices could lure physicians away from offi ces
with traditional insurance arrangements, creating new
areas of shortage, especially for Medicaid enrollees.
16
Because this model supports smaller patient panels,
more physicians are required to see the same number
of people.
17
In fact, if every primary care physician in Colorado
were to adopt the Direct Primary Care approach, the
state would need 4,400 more physicians to make up
for the smaller patient panels.
18
Adoption of the model
would likely never reach this level, but in a profession
already facing shortages, the prospect of losing further
capacity has some providers worried.
19
Dr. Mark Tomasulo, founder of PeakMed, which runs
a number of Direct Primary Care practices, says that
while there could be a short-term impact on physician
numbers, in the longer term he believes the personal
I believe the only way
to do primary care
sustainably for me is
Direct Primary Care.
I think it’s worth the
money, but I want my
patients to think it’s
worth it.”
By Brian Clark, CHI
8 Colorado Health Institute
Primary Care framework. While it is illegal for a
Direct Primary Care doctor to charge a Medicaid
member for services, some operators run a parallel,
traditional practice that takes insurance of all
types, including Medicaid and Medicare. Others
say they reserve a percentage of their patient load
for “charity care” and see Medicaid and uninsured
patients pro-bono.
22
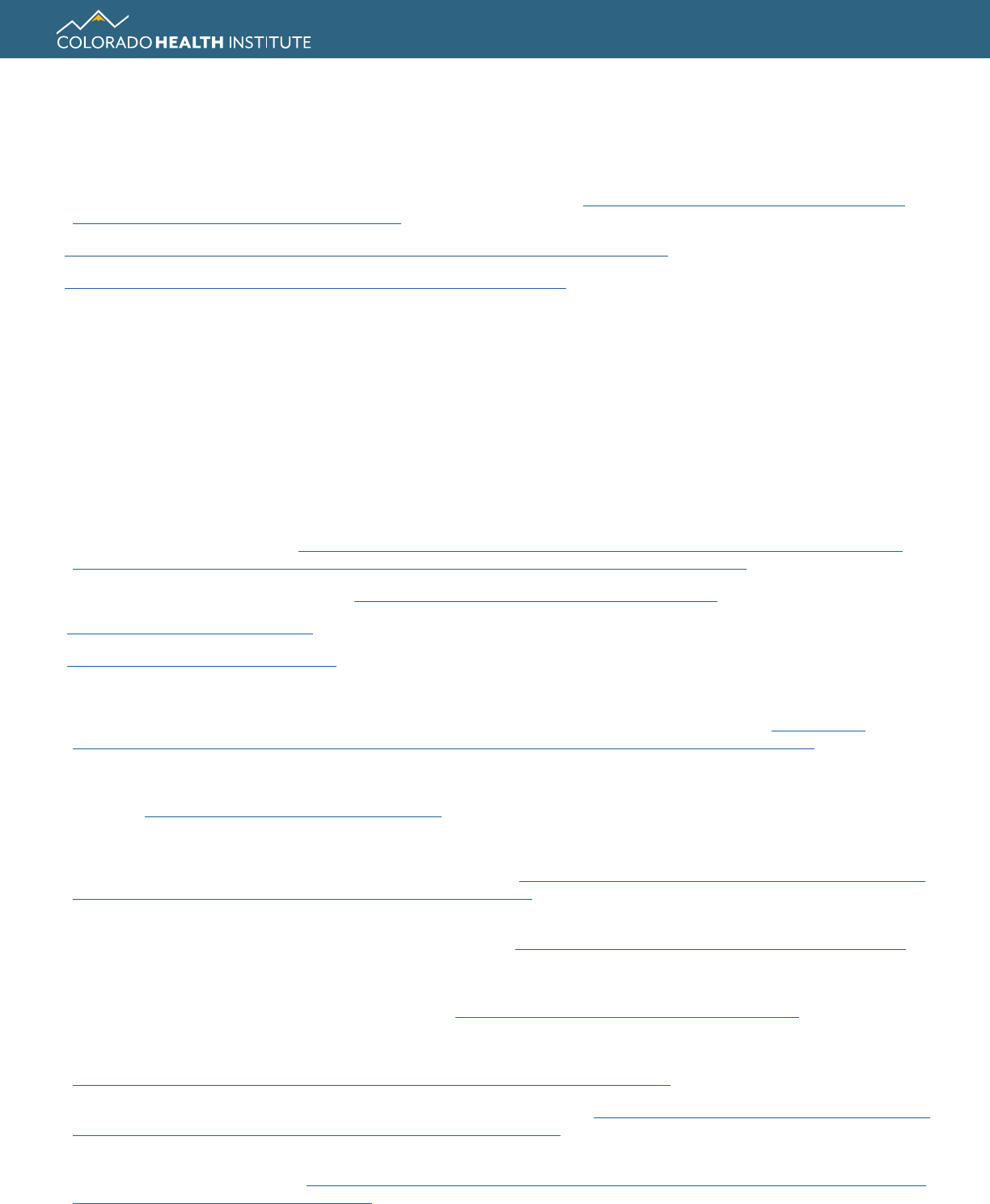
Two Providers, Two Perspectives
Two physicians interviewed by
CHI have different takes on Direct
Primary Care.
Dr. Mark Tomasulo founded
PeakMed as a single Direct
Primary Care clinic in Colorado
Springs in 2014. It now has
multiple sites, a mobile clinic
and house calls. It also has won
contracts with several big Colorado employers,
including school districts and Goodwill Industries.
Dr. Tomasulo believes his clinic is revolutionizing
how employers purchase health care for their
employees. Companies pay PeakMed a per
capita amount based in part on the health of their
employees. For example, a company with a sizable
number of employees with diabetes might receive
a quote that includes access to insulin and A1C
testing for no out-of-pocket cost for the patient.
PeakMed can also target patients who frequently
use emergency rooms and manage their care to
keep them away from high-cost
services like those associated
with uncontrolled diabetes or
other chronic diseases.
But other providers are
skeptical. Among them is
Dr. Mike Pramenko, a family
physician in Grand Junction,
whose clinic serves many
Medicaid members. He worries that Direct Primary
Care will siphon off patients and clinicians alike,
reducing the number of traditional health care
providers, especially those who serve publicly
insured patients.
“We’re playing by the rules,” Dr. Pramenko said.
“We serve low-income individuals, bill Medicaid
and take care of our patients. But we’re losing
providers to the allure of Direct Primary Care. I can
understand why the lifestyle is appealing, but I wish
we could coexist without putting our vulnerable
populations at risk.”
Dr. Tomasulo Dr. Pramenko
and professional benefi ts of Direct Primary Care could
reduce physician burnout, keeping them practicing
longer and attracting more doctors to primary care.
Swapping a high quantity of interactions for high
quality interactions with patients could be a boon to
primary care providers, he says.
Would it create a “two-tiered” health care system?
The departure of doctors from traditional primary care
to Direct Primary Care could exacerbate disparities in
access to health care based on race/ethnicity. Evidence
suggests providers using a subscription model on
average see fewer African-American, Hispanic or
Medicaid patients.
20
Medicare enrollees may also be
affected, since most clinics opt out of offering to care
for them due to red tape.
21
Some clinics in Colorado try to address this by seeing
patients who are publicly insured outside of the Direct
Colorado would need
4,400
More Physicians
If every primary care
physician in Colorado
were to adopt the Direct
Primary Care model.
Colorado Health Institute 9
JUNE 2018
Direct Primary Care: A New Way to Deliver Health Care
How could it affect Health First Colorado
(Medicaid) enrollees?
The American Academy of Family Physicians and
the Colorado Commission on Affordable Health
Care have both recommended pilot programs to
allow Medicaid members to use Direct Primary
Care clinics.
23,24
To date, no efforts have been
made to allow such a program, although some
physicians are expressing interest in a test run.
They believe a pilot could save the state Medicaid
program money by keeping Medicaid patients
healthier and avoiding costly medical expenses.
Conclusion
Direct Primary Care has received a lot of attention as
health care leaders consider how to fi x a primary care
system that often features high insurance prices, low
satisfaction for both patients and providers, and less-
than-optimal health results.
Ever-increasing health care costs have some wondering
if Direct Primary Care could be a solution for delivering
effi cient primary care in Colorado. But could it leave
behind at-risk populations and the clinics serving them?
It will be important for Colorado to weigh the potential
outcomes.
10 Colorado Health Institute
1
Colorado Health Institute analysis of Colorado Direct Primary Care clinics.
2
Colorado Revised Statues Title 25.5: Health Care Policy and Financing 25.5-4-301. http://codes.fi ndlaw.com/co/title-255-health-care-
policy-and-fi nancing/co-rev-st-sect-25-5-4-301.html
3
https://www.kevinmd.com/blog/2014/08/direct-primary-care-concierge-medicine-theyre.html
4
http://www.latimes.com/health/la-he-concierge-medicine-20170114-story.html
5
Colorado Health Institute analysis of Colorado Direct Primary Care clinics.
6
Colorado Health Access Survey, 2017.
7
Colorado Health Institute analysis of Colorado Direct Primary Care clinics.
8
Alexander GC, Kurlander J, Wynia MK. “Physicians in Retainer (“Concierge”) Practice. A National Survey of Physician, Patient, and
Practice Characteristics.” Journal of General Internal Medicine, 2005;20(12):1079–1083
9
Colorado Health Institute analysis of Colorado Direct Primary Care clinics.
10
Connect for Health Colorado: Premium data for 40-year-olds, 2017
11
PR Newswire. “Paladina Health, UnitedHealthcare and State of Colorado Partner to Provide Innovative Physician-Led Primary Care to
State Employees.” January 13, 2016. https://www.prnewswire.com/news-releases/paladina-health-unitedhealthcare-and-state-of-
colorado-partner-to-provide-innovative-physician-led-primary-care-to-state-employees-300203491.html
12
Paladina Health. “Your Available Locations.” https://www.paladinahealth.com/clients/state-colorado. Accessed May 15, 2017.
13
https://leg.colorado.gov/bills/hb17-1115
14
https://nexterahealthcare.com/locations/
15
Colorado Health Access Survey, 2017.
16
Wu, WN et al. “A Direct Primary Care Medical Home: The Qliance Experience.” Health Affairs 36(5). (May 2017). http://content.
healthaffairs.org/content/29/5/959.full?ijkey=5faaf28d6606e333829de56c2320df8d3d4f582e&keytype2=tf_ipsecsha. Accessed May
16, 2017.
17
Weisbart, E. “Is Direct Primary Care the Solution to Our Health Care Crisis?” (September-October 2013). Family Practice Management
23(5); 10-11. http://www.aafp.org/fpm/2016/0900/p10.html. Accessed May 16, 2017.
18
CHI calculated this number using CHAS data and average panel sizes for traditional and Direct Primary Care providers.
19
Robert Graham Center, Colorado: Projecting Primary Care Workforce, https://www.graham-center.org/content/dam/rgc/documents/
maps-data-tools/state-collections/workforce-projections/Colorado.pdf
20
Alexander, GC et al. “Physicians in Retainer (“Concierge”) Practice. A National Survey of Physician, Patient, and Practice
Characteristics.” Journal of General Internal Medicine (2005)20: 1079. https://link.springer.com/article/10.1111/j.1525-1497.2005.0233.x.
Accessed May 16, 2017.
21
Eskew, PM et al. “Direct Primary Care: Practice Distribution and Cost Across the Nation.” Journal of the American Board of Family
Medicine (November-December 2015) 28(6). Pages 793-801. http://www.jabfm.org/content/28/6/793.full.pdf+html. Accessed May 15,
2017.
22
Colorado Department of Health Care Policy and Financing. Policy Statement: Billing Health First Colorado Members for Services.
https://www.colorado.gov/pacifi c/hcpf/policy-statement-billing-medicaid-members-services. Accessed May 14, 2018
23
Colorado Commission on Affordable Health Care. 2017 Final Report. June 30, 2017. https://www.colorado.gov/pacifi c/sites/default/fi les/
Cost%20Commission%20November%202017%20report%20v3%20draft_1.pdf
24
Letter to Bill Lindsay, Colorado Commission on Affordable Health Care, from Tamaan Osbourne-Roberts, Colorado Academy of
Family Physicians. February 24, 2017. https://www.colorado.gov/pacifi c/sites/default/fi les/CAFP_DPC%20Recommendations%20to%20
Cost%20Commission%20February%202017.pdf
Endnotes

Colorado Health Institute 11
JUNE 2018
Direct Primary Care: A New Way to Deliver Health Care

12 Colorado Health Institute
The Colorado Health Institute is a trusted source of independent
and objective health information, data and analysis for the state’s
health care leaders. The Colorado Health Institute is funded by the
Caring for Colorado Foundation, Rose Community Foundation,
The Colorado Trust and the Colorado Health Foundation.
303 E. 17th Ave., Suite 930, Denver, CO 80203 • 303.831.4200
coloradohealthinstitute.org
OUR FUNDERS
