This is a prepress version of the statement that will appear in final form in AJHP at a future
date. That statement will replace this preliminary version when it is final.
ASHP Statement on the Role of Pharmacists in Primary Care
Position
ASHP believes that pharmacists have a role in meeting the primary care needs of patients
directly and in collaboration with other healthcare providers. Primary care pharmacy practice is
the provision of integrated, accessible healthcare services by pharmacists who are accountable
for addressing medication needs, developing sustained partnerships with patients, and
practicing in the context of family and community.
1
Primary care pharmacy practice is
accomplished through the provision of direct patient care and medication management
services (MMS) for ambulatory patients, development of long-term relationships, coordination
of care, patient advocacy, wellness and health promotion, triage and referral, and patient
education and self-management. The primary care pharmacist provides primary care services in
a variety of settings, including institutional, private, and community-based clinics. Primary care
pharmacists help offset deficits in the primary care workforce caused by a shortage of
physicians and other healthcare providers, particularly for underserved populations, by
providing MMS in interdisciplinary team-based settings as well as in areas such as telehealth,
population health, transitions of care, employer-based services, lifestyle medicine, accountable
care organizations, and public health. Primary care pharmacists are often embedded into the
primary care practice to provide MMS.
Many states allow pharmacists to partner with physicians via collaborative practice
agreements (CPAs) that enable physicians to delegate specific tasks (e.g., initiation, titration,
and discontinuation of medications; laboratory monitoring of therapy; medication and disease
state monitoring) to a pharmacist. ASHP supports passage of federal and state laws and
regulations that authorize pharmacists as providers within collaborative practice and that
facilitate reimbursement for services provided by pharmacists.
2
Further, ASHP advocates that
pharmacists be recognized as providers in federal, state, and third-party payment programs.
Provider recognition would facilitate direct billing for services provided, similar to billing by
physicians, nurse practitioners, clinical nurse specialists, and physician assistants.
3
Until that

ASHP Statement on the Role of Pharmacists in Primary Care 2
recognition is obtained, ASHP encourages healthcare organizations to use a variety of models to
ensure the financial sustainability of services provided by primary care pharmacists, such as
through indirect funding, incident-to billing, and increased use of the limited direct insurance
billing opportunities available. Several states have passed pharmacist provider status laws or
reimbursement parity laws allowing for reimbursement for direct patient care pharmacist
services by state Medicaid and/or commercial plans.
4
As pharmacists become core members of the primary care workforce, credentialing and
privileging with payers and healthcare organizations will be essential. As credentialed providers,
pharmacists are able to both provide patient care services and contribute to the financial
sustainability of those services. Privileging protects their employing organizations from legal risk
and ensures patients receive care from qualified and competent providers. ASHP recommends
the use of credentialing and privileging in a manner consistent with other healthcare
professionals to assess a pharmacist’s competence to engage in patient care services.
5
Credentialing and privileging systems already exist for physicians, physician assistants, and
nurse practitioners, but are far less common for pharmacists. Integration of pharmacists into
existing processes will enable the profession to function collaboratively and in parallel with
their colleagues and assist in preparing for pharmacist provider status. There are many
opportunities for pharmacists who practice in primary care settings to seek additional
credentials beyond a pharmacy degree and licensure, and certain credentials may be required
to obtain specific privileges to provide MMS. The variety of state requirements to provide
primary care pharmacist services can be a barrier to patient access to those services, thus
standardized credentialing is needed.
Primary healthcare
A 2021 National Academies of Science, Engineering and Medicine report defined high-quality
primary care as “the provision of whole-person, integrated, accessible, and equitable health
care by interprofessional teams that are accountable for addressing the majority of an
individual’s health and wellness needs across settings and through sustained relationships with
patients, families, and communities.”
6
The report stated that high-quality primary care is a

ASHP Statement on the Role of Pharmacists in Primary Care 3
critical component to achieving the quadruple aims of healthcare: enhancing the patient
experience, improving population health, reducing costs, and improving the health care team
experience.
6
Primary healthcare is a comprehensive and holistic care approach to health and well-being
that is centered on and tailored to the needs of individuals, families, and communities. The
World Health Organization (WHO) has developed a three-component definition of primary care:
1. Meeting people’s health needs through comprehensive promotive, protective,
preventive, curative, rehabilitative, and palliative care throughout the life cycle,
prioritizing key healthcare services aimed at individuals/families through primary care
and the population through public health functions as the central elements of
integrated health services.
2. Systematically addressing the determinants of health (social, economic, environmental,
as well as people’s characteristics and behaviors) through evidence-informed public
policies and actions across all sectors.
3. Empowering individuals, families, and communities to optimize their health, as
advocates for policies that promote and protect health and well-being, as co-developers
of health and social services, and as self-carers and care-givers to others.
7
Primary care pharmacy practice is the provision of integrated, accessible healthcare services by
pharmacists who are accountable for addressing medication needs, developing sustained
partnerships with patients, and practicing in the context of family and community.
1
This
practice is accomplished through direct patient care and medication management for
ambulatory patients, development of long-term relationships, coordination of care, patient
advocacy, wellness and health promotion, triage and referral, and patient education and self-
management. The primary care pharmacist may practice in institutional, private, and
community-based clinics involved in the provision of direct care to diverse patient populations.
Services provided by primary care pharmacists
Primary care pharmacists may help to offset deficits in the primary care workforce, including
the physician shortage, by providing MMS in interdisciplinary team-based settings as well as

ASHP Statement on the Role of Pharmacists in Primary Care 4
areas such as telehealth, population health, transitions of care, employer-based services,
lifestyle medicine, and public health. Clinical pharmacy services may include:
• Immunizations and travel vaccines.
• Medication therapy management (MTM).
• Collaborative drug therapy management (CDTM).
• Comprehensive medication management (CMM).
• Focused specialty management of chronic diseases (e.g., anticoagulation, diabetes,
heart failure).
• Management of complex acute conditions or exacerbation of chronic conditions (e.g.,
urinary tract infection, chronic obstructive pulmonary disease, asthma).
• Provision of personalized medicine (e.g. pharmacogenomics)
• Patient counseling, education, and training.
Examples of practice settings in which pharmacists provide primary care services include:
• Accountable care organizations (ACOs)
• Community-based or free clinic
• Community pharmacy
• Federally Qualified Health Center (FQHC)
• Hospital-based outpatient clinic
• Indian Health Service clinic
• Managed care integrated system
• Outpatient clinic associated with academic medical center
• Patient-centered medical home (PCMH)
• Private practice physician clinic
• Rural health clinic (RHC)
• Self-insured employee clinic
• Veterans Affairs (VA) medical center

ASHP Statement on the Role of Pharmacists in Primary Care 5
MMS. Primary care pharmacists are often embedded into the primary care practice to
provide MMS. MMS has been defined by the Joint Commission of Pharmacy Practitioners (JCPP)
as “a spectrum of patient-centered, pharmacist-provided, collaborative services that focus on
medication appropriateness, effectiveness, safety, and adherence with the goal of improving
health outcomes.”
8
For the purposes of this statement, MMS “encompasses a variety of terms,
such as medication therapy management (MTM), comprehensive medication management
(CMM), and collaborative medication management,” as in the JCPP definition.
3
The pharmacist
may be an employee of the practice, a department of pharmacy, or a health professions school
or college, and may dedicate a part- or full-time effort to providing clinical pharmacy services.
Care may be provided face-to-face or via telehealth visits to manage medications for patients
with chronic illnesses such as hypertension, diabetes, chronic heart failure, asthma, chronic
obstructive pulmonary disease, anticoagulation, osteoporosis, and many others. Primary care
pharmacists often provide patient education about lifestyle choices or conduct annual wellness
visits (AWVs) for patients with Medicare. Many states allow pharmacists to collaborate with
physicians through CPAs that enable physicians to delegate specific tasks such as medication
initiation, titration, or discontinuation; laboratory monitoring of drug therapy; and referral for
medication and disease state management to the pharmacist.
Transitions of care services. The term transitions of care refers to the movement of
patients between healthcare practitioners, settings, and home as their condition and care
needs change.
9
During transitions, medication regimens are frequently changed and may
include medication discontinuation, dosage changes, and new prescriptions that can be
confusing for patients and caregivers to manage. Poor-quality transitions contribute to
medication errors, hospital readmissions, and increased healthcare costs.
9
Pharmacists in the
primary care setting can support patients and caregivers as they adjust to new diagnoses, care
plans, and medications.
Established Transitional Care Management (TCM) Current Procedural Terminology (CPT)
codes allow for billing of transitions of care services, providing a mechanism for
reimbursement.
10,11
There are three required elements to bill for TCM services:

ASHP Statement on the Role of Pharmacists in Primary Care 6
1. Interactive communication (e.g., phone, text, email) must occur with the patient
or caregiver within 2 days of discharge by a licensed clinical staff member, which
can be the primary care pharmacist.
2. Medical decision making of moderate to high complexity occurs during the
service period.
3. The patient has a face-to-face or telehealth visit within 7-14 days of discharge.
Services during TCM visits often include reviewing medical records, reconciling medications,
coordinating future visits, and providing patient education. Pharmacists may be involved with
all components of TCM, but the services can only be billed by a physician or a qualified
nonphysician provider such as a nurse practitioner or physician assistant according to current
Centers for Medicare & Medicaid Services (CMS) rules. Inclusion of pharmacists in the definition
of a nonphysician provider would allow pharmacists to perform these services, among others,
and reduce the burden on primary care providers.
ASHP and the American Pharmacists Association (APhA) collaborated to develop the
Medication Management in Care Transitions (MMCT) Best Practices that spotlight transitions of
care models in pharmacy practice and provide resources for pharmacy leaders.
12
Successful
programs improved patient satisfaction scores and decreased readmission rates and
medication discrepancies.
12
A descriptive study that evaluated the impact of care transitions
intervention on clinical, organizational, and financial outcomes found that adding a pharmacist
to the care transitions team decreased hospital readmissions compared to usual care (9 vs.
26%) and prevented 103 admissions per year, translating to an annual savings of over $1
million.
13
Services offered through employer-based health plans. Employers may offer chronic
disease management or healthy lifestyle programs to employees as part of their human
resources benefits package. Pharmacists are essential team members who can provide chronic
disease medication management to employees enrolled in self-insured health plans. The
Asheville Project demonstrated that pharmacists who cared for City of Asheville employees
with diabetes improved patient satisfaction with their healthcare, decreased healthcare costs,
and increased the number of patients who achieved hemoglobin A1c, lipid, and blood pressure

ASHP Statement on the Role of Pharmacists in Primary Care 7
goals.
14
An evaluation of a national employer-based program offered by 10 organizations in 70
different communities indicated that pharmacists improved other diabetes-related population
health metrics, including monofilament examinations, annual dilated eye examinations, foot
self-exams, glucose self-monitoring, weekly exercise, and annual influenza vaccines.
15
Population health services. A shift to population health strategies in primary care has
been driven by increasing healthcare costs, emphasis on fee-for-service over value-based care,
and lack of widespread prevention initiatives. Primary care pharmacists who dedicate their time
to population health management focus on improving the quality of care for specific patient
populations. Specific population health metrics that warrant improvement are identified by
leaders within the PCMH, the ACO, through community health assessments, or by payers such
as Medicare, Medicaid, and private insurers. Demonstration in improved quality metrics may be
linked with pay-for-performance payment bonuses, or shared savings incentives. For example,
if a metric of importance to the practice is to improve the quality of care for patients with
diabetes, primary care pharmacists can provide MMS for high-risk patients to improve
attainment of hemoglobin A1c goals.
16
Public health services. Expertise in the domain of public health is increasingly important
for the primary care pharmacist due to the impact of public care challenges such as the opioid
epidemic, unintended pregnancy with resultant negative maternal fetal outcomes, tobacco
abuse, and the COVID-19 pandemic. The Opioid and Naloxone Education (ONE) program has
demonstrated the ability of pharmacists to ensure safe opioid use, and prevent opioid misuse
and abuse, through implementing naloxone prescribing while utilizing the pharmacist’s patient
care process.
17
A growing number of states allow pharmacists to prescribe hormonal
contraception as a strategy to increase access to care and decrease negative maternal
outcomes.
18
Oregon pharmacists prescribing hormonal contraception prevented 51 unintended
pregnancies and saved Oregon Medicaid over $1.6 million.
19
As of February 2021, six states
(Idaho, Colorado, Indiana, West Virginia, Vermont, North Dakota, and New Mexico) have
authorized pharmacists to prescribe all FDA-approved tobacco cessation products, including
varenicline, to combat the negative impact of smoking on public health; Oregon and North
Dakota are currently developing regulations to implement authorizing legislation.
20

ASHP Statement on the Role of Pharmacists in Primary Care 8
Pharmacists in primary care settings are also well-positioned to identify immunization
needs of patients, provide education to promote vaccine confidence, and administer vaccines.
During the COVID-19 pandemic, the U.S. Department of Health and Human Resources
authorized immunizing pharmacists to administer childhood vaccines
21
and COVID-19
vaccines
22
as part of the Public Readiness and Emergency Preparedness (PREP) Act.
Telehealth. The Health Resources and Services Administration (HRSA) defines telehealth
as “the use of electronic information and telecommunication technologies to support long-
distance clinical health care, patient and professional health-related education, health
administration and public health.”
23
Telehealth has been used for a variety of patient
populations, including veterans, rural patients, and patients with psychiatric conditions. The
COVID-19 pandemic accelerated the delivery of primary care services by telehealth. The federal
government established temporary measures in 2020 to increase access to telehealth during
the pandemic through the Coronavirus Preparedness and Response Supplemental
Appropriations Act. In addition, CMS relaxed rules for supervision of auxiliary personnel to
allow physicians to provide “virtual” supervision in order to promote social distancing and
protect frontline healthcare workers.
Telehealth visits may be billed by physicians and nonphysician providers and are paid at
the same fee-for-service rate as in-person visits for Medicare recipients. Pharmacists may be
able to bill using certain approved telephone codes. Reimbursement may vary for Medicaid
and private insurance.
Special practice settings and patient populations
Rural health. Rural areas make up approximately 97% of the land area in the U.S., yet
account for just a little over 19% of the total U.S. population.
24
People living in rural areas are
often underserved and experience significant health disparities that can vary between
geographical regions and across socioeconomic spectra. Many of the health-related challenges
faced by rural America are amplified by the lack of adequate services, particularly primary care
providers and medical specialists. Approximately 90% of Americans live within 5 miles of a

ASHP Statement on the Role of Pharmacists in Primary Care 9
community pharmacy, creating additional opportunities for pharmacists to partner with
primary care providers and provide clinical pharmacy services for rural, underserved patients.
25
The expansion of pharmacist-delivered services in rural settings is an important strategy
to target health disparities that are more common causes of mortality for people who live in
rural communities than those living in urban areas. Chronic disease state management, MMS,
health screenings, tobacco cessation management and prescribing, medication-assisted
treatment of opioid use disorders, and lifestyle coaching through diabetes prevention programs
are examples of services that address these common health disparities and can be led by
pharmacists or enhanced through interprofessional collaboration with pharmacists as allowed
under state-specific pharmacy practice acts. Unique training programs focused on rural
pharmacy health exist at several colleges of pharmacy that focus on preparing pharmacists for
leadership roles in small and rural communities.
26
Many health systems that serve rural America receive reimbursement through all-
inclusive payment models by Medicare and many state bill Medicaid plans. However, the lack of
pharmacist recognition as an independent billable provider by the majority of payers, including
Medicare, can challenge the financial feasibility of advanced pharmacist services within these
settings.
27
Pharmacists can assist or serve a key role in grant-funded projects and programs and,
in the case of government-funded grants, can lead to perpetual funding to rural health
providers such as FQHCs, RHCs, and the Indian Health Service as a mechanism to defray
pharmacist costs. Examples of sustainable practice models that incorporate pharmacist-
delivered care in rural areas include the following:
1. Synchronous or co-visits between a pharmacist and a primary care practitioner who is
recognized as an independent billable provider.
2. Visits with a pharmacist independent of other health professionals.
3. Pharmacist involvement in comprehensive care services as part of the PCMH or
ambulatory primary care clinic care team.
4. Population health services that focus on quality improvement and can increase
reimbursement to the health system or collaborating primary care provider through
individual visits with the pharmacist face-to-face or via telehealth, including remote

ASHP Statement on the Role of Pharmacists in Primary Care 10
physiologic monitoring (examples of quality improvement measures include blood
pressure control, warfarin monitoring, glycemic control, rates of influenza
immunizations, and adherence to medication refills [e.g., statin therapy, antiplatelet
medications, oral glucose-lowering medications]).
5. Pharmacists involved in accredited Diabetes Self-Management Training (DSMT)
programs.
Partnerships between primary care providers and local community pharmacies, critical access
pharmacies, or academic institutions can increase access to essential services such as
immunization delivery, point-of-care testing, and disease state education and management to
people living in rural areas with limited access to primary care providers.
28-30
FQHCs. FQHCs are considered safety net health providers of outpatient clinical services
that receive funding from the HRSA Health Center Program to provide care to individuals in
underserved areas.
31
The primary purpose of FQHCs is the provision of primary care services in
underserved urban and rural communities. FQHCs are typically located in community health
centers but are also found in public housing primary care centers, outpatient health programs
operated by a tribe or urban Indian organization, migrant health centers, and healthcare for the
homeless centers. Among the requirements of FQHCs are the provision of a sliding fee scale
system for uninsured patients with incomes below 200% of the federal poverty guidelines,
provision of comprehensive healthcare services (which include medical, pharmacy, dental, and
behavioral health), an ongoing quality assurance program, and a governing board of directors.
32
FQHCs often need to meet the challenges of geographic, social, economic, linguistic, and
cultural patient barriers. Primary care pharmacists working in clinical roles within an FQHC can
have a tremendous impact on the care of this underserved patient population. Socioeconomic
and cultural/language barriers present unique challenges to medication therapy that
pharmacists are well suited to help overcome. Chronic diseases are common, noting a high
prevalence of hypertension, diabetes and tobacco use. The Uniform Data System requires
FQHCs to report on quality of care measures, therefore providing an opportunity for
pharmacists to assist in the design and implementation of clinical services aimed at meeting
quality benchmarks, as well as participate in the reporting process.

ASHP Statement on the Role of Pharmacists in Primary Care 11
FQHCs differ from traditional primary care practices in the way that payment is issued
for primary care encounters. An encounter payment is issued under the FQHC Prospective
Payment System (PPS) from CMS that includes medical services, supplies, and overall service
coordination provided to patients. The specific payment amount is unique to each FQHC and is
determined based on reasonable costs and cost reporting. Because the PPS is provided through
CMS, only practitioners who are recognized as healthcare providers by Medicare are eligible to
bill directly for services. Because pharmacists are not recognized as healthcare providers
federally, any eligible services provided by a pharmacist may not be billed directly but must
rather be billed by an eligible healthcare provider. Despite the limited opportunities for
pharmacists to promote sustainability through direct revenue, such as Medicare AWVs, there
are many primary care services provided by pharmacists in FQHCs that benefit the practice.
FQHCs that participate in the 340B program, which provides medication cost savings to
uninsured and underinsured patients as well as savings to the pharmacy, commonly leverage
the savings to support clinical pharmacy services (e.g., hiring or salary support of a clinical
pharmacist). Examples of services provided by pharmacists in FQHCs include:
• MTM
• 340B Program
• Specialty Pharmacy Services
• Spirometry
• Chronic Care Management (CCM) and Principal Care Management (PCM)
• Diabetes Self-Management Training (DSMT)
• Value-Based Care
• Quality Improvement/PCMH
• CDTM/Contract Agreements/Consult Agreements
• Population Health
• Medicare AWVs
• TCM
ASHP Statement on the Role of Pharmacists in Primary Care 12
Additional detailed information can be found in the ASHP Resource Center document,
“Opportunities for Sustainable Pharmacy Services in Federally Qualified Health Centers.”
33
Billing and reimbursement for primary care pharmacy services
The National Academy of Sciences recommends that payers, including Medicaid, Medicare,
commercial insurers, and self-insured employers, should shift payments toward a hybrid model
that includes fee-for-service and capitated payments, and that these models should pay
prospectively for interprofessional, integrated, team-based care.
6
Financial sustainability for
services provided by primary care pharmacists may be achieved using a variety of models. Due
to lack of federal provider status for pharmacists and subsequent inability to directly bill
Medicare as primary care providers, organizations and practices have become creative in
maintaining financial sustainability of primary care pharmacist services. Some settings utilize
indirect funding, while others take advantage of some of the limited direct insurance billing
opportunities to fund pharmacists in primary care settings. Direct billing opportunities will vary
based on the setting, hospital-based versus physician-based practices, as well as state-specific
laws and regulations. Medicare, Medicaid, and commercial health plans may reimburse
pharmacists for certain services, while some will require direct contracting with the health plan.
Several states have passed pharmacist state provider status laws and/or reimbursement parity
laws allowing for reimbursement for direct patient care pharmacist services by state Medicaid
and/or commercial plans.
4
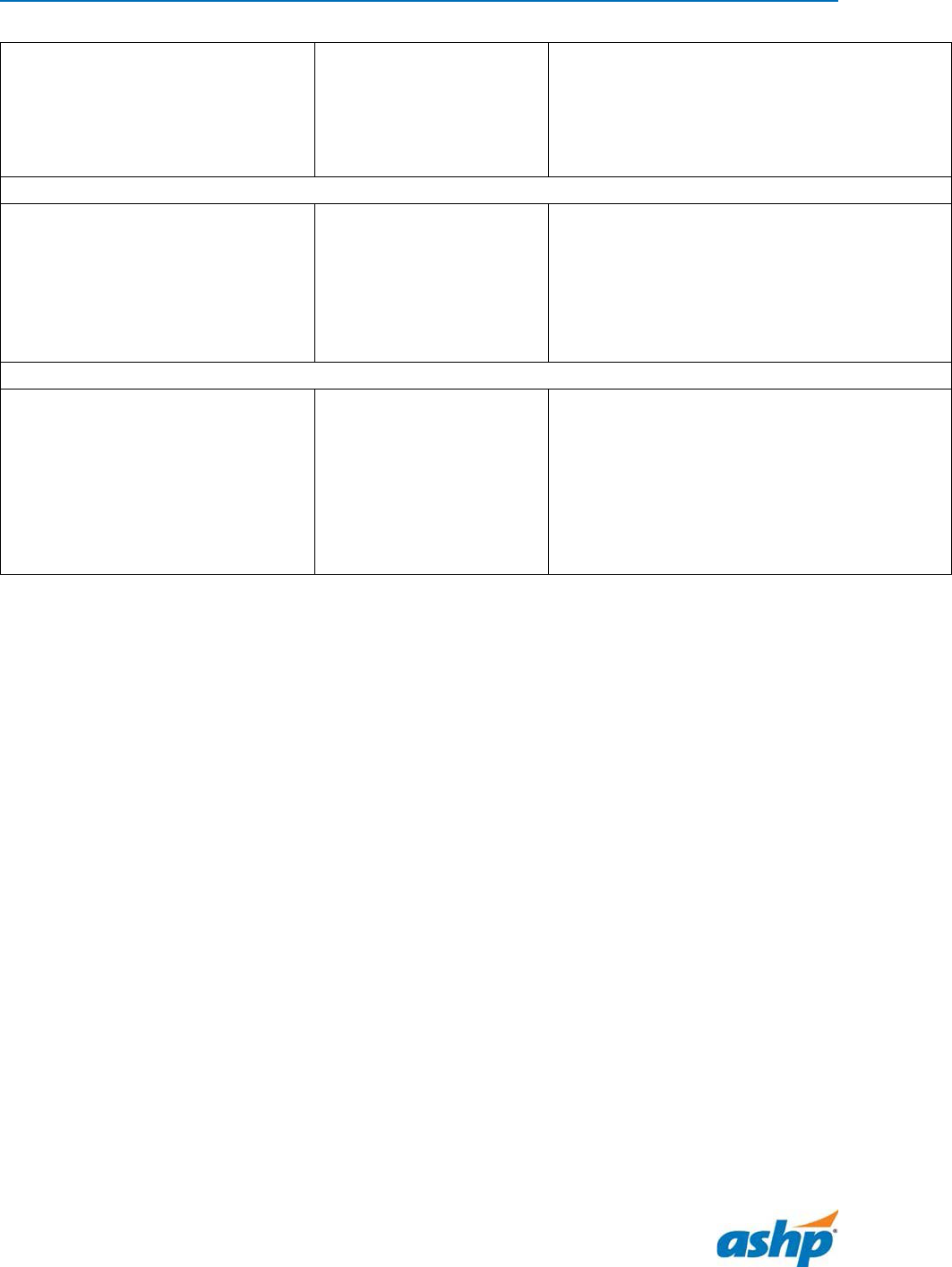
Some examples of direct and indirect billing methods are listed in
Table 1.
ASHP Statement on the Role of Pharmacists in Primary Care 13
Table 1. Examples of direct and indirect funding methods.
34
Indirect billing
Direct billing
Funding by Colleges of Pharmacy/Academic
Health Centers: shared pharmacy practice
faculty in primary care settings
Affordable Care Organizations/Managed Care
Insurance Plans
• Quality improvement/achieving quality
metrics
• Reducing medication adverse
events/improving disease management
340B Drug Program Covered Entities:
Reinvestment of 340B drug cost savings in
salary for clinical pharmacists
35
Medicare Part B/D:
• Annual Wellness Visits
• Chronic Care Management
• Facility Fee Billing (hospital-based
clinics)
36
• Incident-to (physician-based clinics)
37
• MTM contract with Medicare Part D
plans
38
• Transitional Care Management
Medicaid or Commercial Health Plans:
• State law dependent
39,40
Credentialing and privileging
As pharmacists look to fill gaps in the primary care workforce and create financially sustainable
practices, credentialing and privileging with payers and healthcare organizations are essential.
Credentialing and privileging are two separate processes. Credentialing is the process by which
an individual’s credentials (i.e., academic, license, certifications) are verified to reflect that they
have the appropriate training to practice as a pharmacist. Privileging evaluates and authorizes
providers to deliver care within a requested scope of practice. For example, if a pharmacist is
practicing in a specialty clinic such as hematology/oncology, they would have a different scope
than when practicing in a primary care setting. The privileging process ensures individuals have
the training and competency to provide the requested services in a particular specialty. Often
this verification is obtained through a peer evaluation process, whereby colleagues provide
feedback on the provider’s clinical knowledge, skills, and professional performance.

ASHP Statement on the Role of Pharmacists in Primary Care 14
With the expanding roles of pharmacists, growth in specialization, and the increased
complexity of healthcare, the credentialing and privileging process is more important than ever.
Credentialing is required by payers in order for providers to bill for services. As credentialed
providers, pharmacists are able to both provide patient care services and contribute to the
financial sustainability of the service. Privileging protects the organization from legal risk and
ensures patients receive care from qualified and competent providers. These systems already
exist for pharmacists, physician, physician assistant, and nurse practitioner colleagues;
integration of pharmacists into existing processes will enable the profession to function in
parallel and collaboratively with our colleagues and assist in preparing for provider status.
Credentials beyond pharmacy degree and state licensure
There are multiple opportunities for pharmacists who practice in primary care settings to seek
additional credentials beyond the pharmacy degree and licensure, and certain credentials may
be required to obtain specific privileges to provide MMS. For example, pharmacists who
prescribe hormonal contraception or who serve as immunizing pharmacists must complete
training and/or certificate programs to be eligible to provide those services in their state.
Certain requirements must also be met in order to enter into CPAs and vary by state.
Pharmacists who practice under a CPA in New Mexico, California, Montana, and North Carolina
are recognized as Pharmacist Clinician (NM), Advanced Practice Pharmacist (CA), and Clinical
Pharmacist Practitioner (NC and MT). The wide variety of state requirements to provide primary
care pharmacy services serves as a barrier for patient access to services, and advocacy to
standardize credentialing is needed.
Employers may require that primary care pharmacists complete a postgraduate year 1
(PGY1) and/or a PGY2 residency training program. They may also require board certification
through the Board of Pharmacy Specialties or completion of an interprofessional certificate,
such as the Certified Asthma Educator (AE-C), Certified Diabetes Care and Education Specialist
(CDCES, formerly Certified Diabetes Educator or CDE), or Certified Anticoagulation Care
Provider (CACP), among others. A listing of board certification opportunities along with
eligibility criteria for examination are listed in the Appendix. All board certification programs

ASHP Statement on the Role of Pharmacists in Primary Care 15
listed incur an examination fee, and pharmacists must achieve a passing score on the
examination and meet ongoing requirements for renewal. Benefits of board certification
include greater marketability, enhanced confidence, improved competence, increased
responsibility, and a competitive edge in job placement and advancement.
41
The Council on
Credentialing in Pharmacy has established guiding principles for post-licensure credentialing of
pharmacists.
42
Conclusion
There are many avenues in which pharmacists can become involved in primary care practice.
Identifying the ideal practice model and service offering will involve collaboration with other
healthcare providers as well as identifying a patient population and target outcome.
Achievement of federal provider status will allow pharmacists the ability to bill Medicare and
create sustainable services and financial stability, as has been demonstrated in states with
active provider status laws. As pharmacists become more involved in primary care practice,
healthcare will move closer towards the goal of optimal, safe, and effective use of medications
for all people all of the time.
References
1. Donaldson MS, Yordy KD, Lohr KN et al., eds. Primary care: America’s health in a new
era. Committee on the Future of Primary Care, Division of Health Services, Institute of
Medicine. Washington, DC: National Academy Press; 1996.
2. ASHP policy 1715, Collaborative Practice. In: Hawkins B, ed. Best practices: positions and
guidance documents of ASHP. 2020-2021 ed. Bethesda, MD: American Society of
Health-System Pharmacists; 2021. www.ashp.org/Pharmacy-Practice/Policy-Positions-
and-Guidelines/Browse-by-Document-Type/Policy-Positions (accessed August 18, 2021).
3. ASHP policy 1502, Pharmacist Recognition as a Healthcare Provider. In: Hawkins B, ed.
Best practices: positions and guidance documents of ASHP. 2020-2021 ed. Bethesda,
MD: American Society of Health-System Pharmacists; 2021. www.ashp.org/Pharmacy-
Practice/Policy-Positions-and-Guidelines/Browse-by-Document-Type/Policy-Positions
(accessed August 18, 2021).
4. National Alliance of State Pharmacy Associations. 2021 State Provider Status Mid-Year
Legislative Update (June 7, 2021). https://naspa.us/2021/06/2021-state-provider-status-
mid-year-legislative-update/ (accessed 15 Dec 2021).
5. ASHP policy 2011, Credentialing and Privileging by Regulators, Payers, and Providers of
Collaborative Practice. In: Hawkins B, ed. Best practices: positions and guidance

ASHP Statement on the Role of Pharmacists in Primary Care 16
documents of ASHP. 2020-2021 ed. Bethesda, MD: American Society of Health-System
Pharmacists; 2021. www.ashp.org/Pharmacy-Practice/Policy-Positions-and-
Guidelines/Browse-by-Document-Type/Policy-Positions (accessed August 18, 2021).
6. National Academies of Sciences, Engineering, and Medicine 2021. Implementing High-
Quality Primary Care: Rebuilding the Foundation of Health Care. Washington, DC: The
National Academies Press. https://doi.org/10.17226/25983.
7. World Health Organization. Primary health care. https://www.who.int/news-room/fact-
sheets/detail/primary-health-care (accessed August 20, 2021).
8. Joint Commission of Pharmacy Practitioners. Medication management services
definition and key points (March 14, 2018). https://jcpp.net/wp-
content/uploads/2018/05/Medication-Management-Services-Definition-and-Key-
Points-Version-1.pdf (accessed August 20, 2021).
9. The Joint Commission. 2012. Transitions of Care: The need for a more effective
approach to continuing patient care – Hot Topics in Health Care, Issue No. 1.
10. Cavanaugh J, Olson J, Parrott AM. Billing for transitional care management visits (2018).
https://www.ashp.org/-/media/assets/pharmacy-practice/resource-
centers/ambulatory-care/transitional-care-management-codes.ashx (accessed August
20, 2021).
11. Medicare Learning Network. Transitional Care Management Services (Publication
MLN908628, July 2021). https://www.cms.gov/Outreach-and-Education/Medicare-
Learning-Network-MLN/MLNProducts/Downloads/Transitional-Care-Management-
Services-Fact-Sheet-ICN908628.pdf (accessed January 31, 2022).
12. American Society of Health-System Pharmacists, American Pharmacists Association.
ASHP-APhA Medication Management in Care Transitions Best Practices (2013).
https://www.ashp.org/-/media/assets/pharmacy-practice/resource-centers/quality-
improvement/learn-about-quality-improvement-medication-management-care-
transitions.ashx (accessed August 20, 2021).
13. Cavanaugh J, Pinelli N, Eckel S et al. Advancing Pharmacy Practice through an Innovative
Ambulatory Care Transitions Program at an Academic Medical Center. Pharmacy. 2020;
8:40.
14. Garrett DG, Bluml BM. Patient self-management program for diabetes: first-year clinical,
humanistic, and economic outcomes. J Am Pharm Assoc. 2005; 45:130-7.
15. Bunting BA, Nayyer D, Lee C. Reducing health care costs and clinical outcomes using an
improved Asheville Project model. Innov Pharm. 2015; 6:Article 227.
16. ASHP Section of Ambulatory Care Practitioners Advisory Group on Clinical Practice
Advancement. FAQ: Getting started with population health management (March 2021).
https://www.ashp.org/-/media/assets/pharmacy-practice/resource-
centers/ambulatory-care/population-health-faq.pdf (accessed Sep. 14, 2021).
17. Skoy E, Eukel H, Werremeyer A et al. Implementation of a statewide program within
community pharmacies to prevent opioid misuse and accidental overdose. J APhA. 2020;
60(1):117-21.
18. Rafie S, Landau S. Opening new doors to birth control: state efforts to expand access to
in community pharmacies. Birth Control Pharmacist (2019).
https://birthcontrolpharmacist.com/2019/12/21/report/ (accessed August 20, 2021).

ASHP Statement on the Role of Pharmacists in Primary Care 17
19. Rodriguez MI, Hersh A, Anderson LB et al. Association of pharmacist prescription of
hormonal contraception with unintended pregnancies and Medicaid costs. Obstet
Gynecol. 2019; 133:1238-46.10.
20. National Alliance of State Pharmacy Associations. Pharmacist Prescribing: Tobacco
Cessation Aids (February 10, 2021). https://naspa.us/resource/tobacco-cessation/
(accessed August 19, 2021).
21. Department of Health and Human Services. HHS expands access to childhood vaccines
during COVID-19 pandemic. https://www.hhs.gov/about/news/2020/08/19/hhs-
expands-access-childhood-vaccines-during-covid-19-pandemic.html (accessed August
19, 2021).
22. Department of Health and Human Services. Trump administration takes action to
expand access to COVID-19 vaccines.
https://www.hhs.gov/about/news/2020/09/09/trump-administration-takes-action-to-
expand-access-to-covid-19-vaccines.html (accessed August 20, 2021).
23. Health Resources and Services Administration. Office for the Advancement of
Telehealth. https://www.hrsa.gov/rural-health/telehealth (accessed August 20, 2021).
24. Ratcliffe M, Burd C, Holder K et al. Defining Rural at the U.S. Census Bureau (ACSGEO-1).
Washington, DC: U.S. Census Bureau; 2016.
https://www2.census.gov/geo/pdfs/reference/ua/Defining_Rural.pdf (accessed August
20, 2021).
25. Kelling SE. Exploring accessibility of community pharmacy services. Innov Pharm. 2015;
6: Article 210. https://pubs.lib.umn.edu/index.php/innovations/article/view/392
(accessed August 20, 2021).
26. Scott MA, Kiser S, Park I et al. Creating a new rural pharmacy workforce: Development
and implementation of the Rural Pharmacy Health Initiative. Am J Health Syst Pharm.
2017; 74:2005-12. doi: 10.2146/ajhp160727.
27. Centers for Medicare & Medicaid Services. Medicare Claims Processing Manual, Chapter
9: Rural Health Clinics/ Federally Qualified Health Centers (18 September 2020).
https://www.cms.gov/Regulations-and-
Guidance/Guidance/Manuals/Downloads/clm104c09.pdf (accessed August 20, 2021).
28. Como M, Carter CW, Larose-Pierre M et al. Pharmacist-led chronic care management for
medically underserved rural populations in Florida during the COVID-19 pandemic. Prev
Chronic Dis. 2020; 17:200265. doi: http://dx.doi.org/10.5888/pcd17.200265
29. Department of Health and Human Services, Office of the Secretary. Third amendment to
declaration under the Public Readiness and Emergency Preparedness Act for Medical
Countermeasures Against COVID–19. Fed Reg. 52136 (August 24, 2020). Available at:
https://www.govinfo.gov/content/pkg/FR-2020-08-24/pdf/2020-18542.pdf (accessed
August 20, 2020).
30. Department of Health and Human Services, Office of the Assistant Secretary for Health.
Guidance for licensed pharmacists, COVID-19 testing, and immunity under the PREP Act
(April 8, 2020). https://www.hhs.gov/sites/default/files/authorizing-licensed-
pharmacists-to-order-and-administer-covid-19-tests.pdf (accessed August 20, 2021).

ASHP Statement on the Role of Pharmacists in Primary Care 18
31. Health Resources & Services Administration (HRSA). Federally Qualified Health Centers:
Eligibility. https://www.hrsa.gov/opa/eligibility-and-registration/health-
centers/fqhc/index.html (accessed August 20, 2021).
32. Centers for Medicare & Medicaid Services Medicare Learning Network Booklet.
Federally Qualified Health Center. https://www.cms.gov/Outreach-and-
Education/Medicare-Learning-Network-
MLN/MLNProducts/downloads/fqhcfactsheet.pdf (accessed August 20, 2021).
33. Maack B, Awad M, Rosselli J. Opportunities for Sustainable Pharmacy Services in
Federally Qualified Health Centers (January 2022). https://www.ashp.org/pharmacy-
practice/resource-centers/ambulatory-care/compensation-and-sustainable-business-
models (accessed January 31, 2022).
34. ASHP Ambulatory Care Resource Center: Compensation and Sustainable Business
Models. https://www.ashp.org/Pharmacy-Practice/Resource-Centers/Ambulatory-
Care/Compensation-and-Sustainable-Business-Models. (accessed August 20, 2021).
35. Health Resources & Services Administration Office of Pharmacy Affairs.
https://www.hrsa.gov/opa/index.html (accessed August 20, 2021).
36. Parrott A, Kline E, Renaurer M et al. FAQ: Facility Fee Billing (August 2021).
https://www.ashp.org/-/media/assets/pharmacy-practice/resource-
centers/ambulatory-care/Facility-Billing.pdf (accessed Sep. 14, 2021).
37. Pharmacist Billing/Coding Quick Reference Sheet For Services Provided in Physician-
Based Clinics. https://www.ashp.org/-/media/assets/pharmacy-practice/resource-
centers/ambulatory-care/billing-quick-reference-sheet.ashx (accessed August 20, 2021).
38. Centers for Medicare & Medicaid Services. Medication Therapy Management.
https://www.cms.gov/Medicare/Prescription-Drug-
Coverage/PrescriptionDrugCovContra/MTM (accessed August 20, 2021).
39. New Mexico House Bill 42. Pharmaceutical Reimbursement Parity.
https://www.nmlegis.gov/Legislation/Legislation?Chamber=H&LegType=B&LegNo=42&
year=20 (accessed August 20, 2021).
40. Washington State Engrossed Substitute Senate Bill 5557.
http://lawfilesext.leg.wa.gov/biennium/2015-
16/Pdf/Bills/Senate%20Passed%20Legislature/5557-S.PL.pdf (accessed August 20,
2021).
41. Board of Pharmacy Specialties. Making a difference. https://www.bpsweb.org/impact-
of-bps-certification/making-a-difference/ (accessed August 20, 2021).
42. Council on Credentialing in Pharmacy. Credentialing and privileging of pharmacists. Am J
Health-Syst Pharm. 2014; 71:1891-1900.
Additional information
Developed through the ASHP Section of Ambulatory Care Pharmacists and approved by the
ASHP Board of Directors on February 24, 2022, and by the ASHP House of Delegates on May 19,
2022. This statement supersedes the ASHP Statement on the Pharmacist’s Role in Primary Care
dated June 7, 1999.

ASHP Statement on the Role of Pharmacists in Primary Care 19
Acknowledgments
ASHP gratefully acknowledges the following individuals for reviewing the current version of the
statement (review does not imply endorsement): Jaclyn A. Boyle, Pharm.D., M.B.A., BCACP;
Jamie J. Cavanaugh, Pharm.D., CPP; Christina E. DeRemer, Pharm.D., BCACP, BCPS, TTS, FASHP;
Ashley M. Parrott, Pharm.D., M.B.A., BCPS, BCACP; Jessica W. Skelley, Pharm.D., BCACP; and
Daniel B. Truelove, Pharm.D., BCACP, BCPS. The contributions of Kimberly A. Galt, Pharm.D.,
FASHP; Richard F. Demers; and Richard N. Herrier, Pharm.D.; to the previous version of this
statement are also gratefully acknowledged.
Authors
Melanie A. Dodd, Pharm.D., PhC, BCPS, FASHP
The University of New Mexico College of Pharmacy
Albuquerque, NM
Seena L. Haines, Pharm.D., BCACP, NBC-HWC, CHWC, FNAP, FCCP, FAPhA, FASHP
The University of Mississippi School of Pharmacy
Jackson, MS
Brody Maack, Pharm.D., BCACP, CTTS
North Dakota State University School of Pharmacy
Fargo, ND
Jennifer L. Rosselli, Pharm.D., BCPS, BCACP, BC-ADM, CDCES
Southern Illinois University Edwardsville School of Pharmacy
Edwardsville, IL
SIHF Healthcare
Belleville and O’Fallon, IL
J. Cody Sandusky, Pharm.D.
Harrisburg Medical Center
Harrisburg, IL
Mollie Ashe Scott , Pharm.D., BCACP, CPP, FASHP
UNC Eshelman School of Pharmacy
Asheville, NC
Betsy Bryant Shilliday, Pharm.D., CDCES, CPP, BCACP, FASHP
UNC Health and UNC Faculty Physicians
Chapel Hill, NC
Disclosures
The authors have declared no potential conflicts of interest.
ASHP Statement on the Role of Pharmacists in Primary Care 20
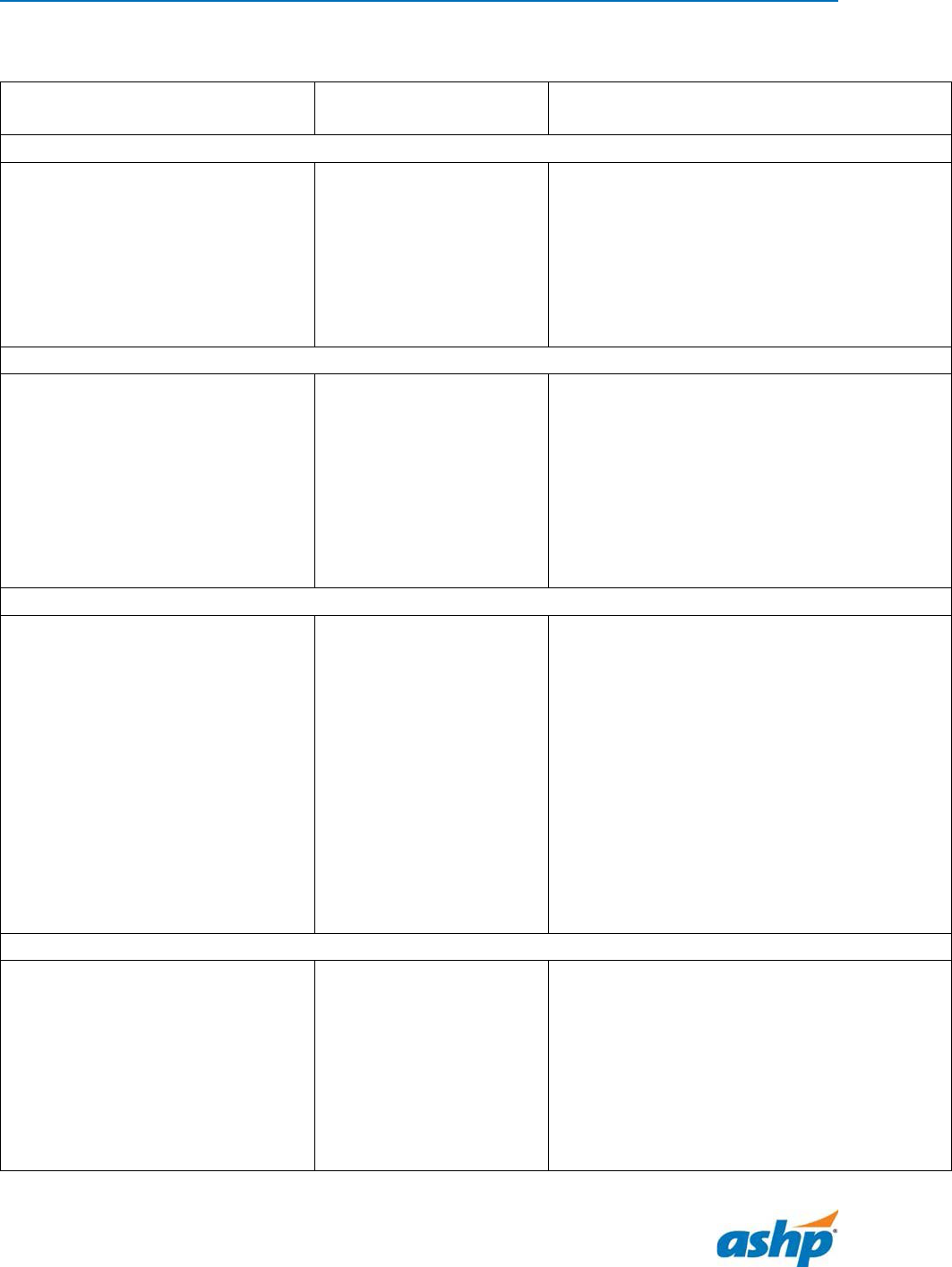
Appendix. Board Certification Opportunities for Primary Care Pharmacists
Credential
Certification Body
Eligibility Criteria for Examination
Ambulatory Care
Board Certified Ambulatory Care
Pharmacist (BCACP)
Board of Pharmacy
Specialties
https://www.bpsweb.or
g/bps-
specialties/ambulatory-
care/
• Graduation from an ACPE accredited
pharmacy program
• Current license to practice
• Demonstration of ambulatory care
practice experience
Anticoagulation
Certified Anticoagulation Care
Provider (CACP)
National Certification
Board for
Anticoagulation Care
Providers
www.ncbap.org
• Must hold professional license for two
years
• Registered nurse, nurse practitioner,
registered pharmacist, physician, or
physician assistant
• 750 hours of active antithrombotic
management within the 18 months
prior to taking the examination
Asthma
Certified Asthma Educator (AE-C)
National Asthma
Educator Certification
Board
https://naecb.com/
• Licensed healthcare professionals such
as pharmacists, physicians, physician
assistants, nurses, respiratory
therapists, pulmonary function
technologists, social workers, health
educators, physical therapists, and
occupational therapists
• Individuals providing direct patient
asthma education, counseling or
coordinating services with a minimum
of 1000 hours experience in these
activities
Diabetes
Board Certified Advanced
Diabetes Management (BC-ADM)
Association of Diabetes
Care and Education
Specialists
https://www.diabetese
ducator.org/education/
certification/bc_adm
• Registered nurse, nurse practitioner,
clinical nurse specialists, registered
dietician, pharmacist, physician
assistant, physician
• 500 clinical practice hours within 48
months of taking the examination
ASHP Statement on the Role of Pharmacists in Primary Care 21
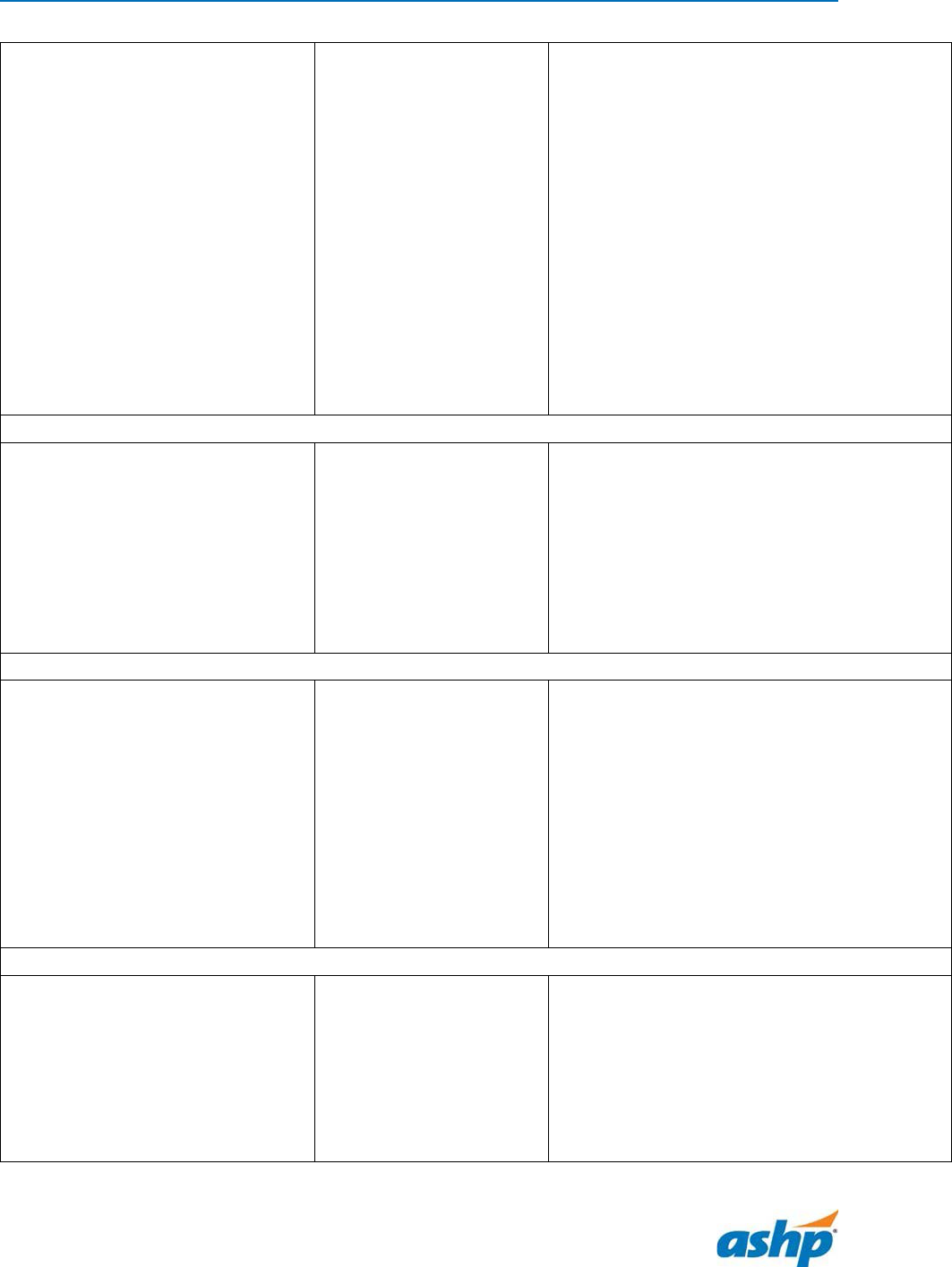
Certified Diabetes Care and
Education Specialist (CDCES)*
Certification Board for
Diabetes Care and
Education
https://www.cbdce.org/
• Qualifying healthcare professional:
registered nurse, nurse practitioner,
registered dietician, pharmacist,
physician assistant, physician, and
others
• 2 years of prior professional experience
• A minimum of 1000 hours providing
diabetes care and education in the
previous 4 years with a minimum of 400
hours in the previous year
• A minimum of 15 hours of approved
continuing education focused on
diabetes in the previous 2 years
Geriatrics
Board Certified Geriatric
Pharmacist (BCGP)
Board of Pharmacy
Specialties
https://www.bpsweb.or
g/bps-
specialties/geriatric-
pharmacy/
• Graduation from an ACPE accredited
pharmacy program
• Current license to practice
• Demonstration of geriatric practice
experience
HIV
HIV Pharmacist (AAHIVP)
American Academy of
HIV Medicine
https://aahivm.org/hiv-
pharmacist/
• Pharmacist licensure
• Documentation of direct HIV care for 25
patients living with HIV within the
preceding 36 months
• Participate in the Academy’s Clinical
Consult Form
• Complete a minimum of 45 credits or
activity hours of HIV and/or HCV-related
continuing education within the
preceding 36 months
Lipids
Clinical Lipid Specialist (CLS)
Accreditation Council
for Clinical Lipidology
https://www.lipidspecia
list.org/certchoose/cls/
• Completed a minimum of 10 continuing
education credit hours in clinical
lipidology in the previous 2 years
• Physicians, nurses, nurse practitioners,
physician assistants, pharmacists,
registered dieticians/nutritionists,
clinical exercise physiologists/specialists
ASHP Statement on the Role of Pharmacists in Primary Care 22
• 2000 hours of demonstrated clinical
experience in the management of
patients with lipid or other related
disorders
• Additional training requirements
Medication Therapy Management
Board Certified Medication
Therapy Management Specialist
(BCMTMS)
The National Board of
Medication Therapy
Management (NBMTM)
https://www.nbmtm.or
g/bcmtms/
• Pharmacy degree
• Pharmacy license
• 2 years of experience in MTM
experience or NBMTM training
Psychiatry
Board Certified Psychiatric
Pharmacist (BCPP)
Board of Pharmacy
Specialties
https://www.bpsweb.or
g/bps-
specialties/psychiatric-
pharmacy/
• Graduation from an ACPE accredited
pharmacy program
• Current license to practice
• Defined practice experiences or PGY2
Psychiatric Pharmacy Residency
*previously the Certified Diabetes Educator (CDE)
Copyright © 2022, American Society of Health-System Pharmacists, Inc. All rights reserved.
